What is Femoroacetabular impingement syndrome?
Femoroacetabular impingement (FAI) syndrome is a movement-related problem of the hip, often leading to pain in the hip or groin region. It is caused by abnormal or premature contact between the top of the thigh bone and the hip socket during movement, or in certain positions.
For the syndrome to be properly diagnosed, three main criteria are required:
- A patient must report symptoms, such as hip or groin region pain, clicking, catching, or giving way
- Certain clinical signs must be present, for instance, reduced range of motion of the hip
- Certain ‘features’ must be seen on x-ray of the hip: usually a ‘cam’ or ‘pincer’ lesion
Anatomy of femoroacetabular impingement syndrome:
The hip is a ball and socket joint. The socket is called the acetabulum and is part of the pelvis. The ball is at the very top of the femur (thigh bone) and is called the ‘head of the femur.’
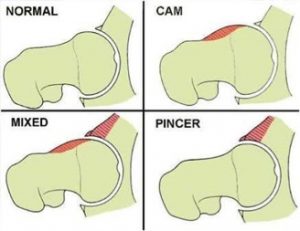
In FAI syndrome, one or two features are seen on x-ray:
- A ‘cam’ shape: a ‘bump’ of bone may be seen at the junction of the ‘head’ and the ‘neck’ of the femur bone, causing an area of convexity
- A ‘pincer’ shape: the acetabulum (socket) has too much coverage or overhang over the top of femur
- A mix of the two features above
These bone features can be responsible for reducing the amount of ‘clearance’ within the hip joint, causing abnormal contact to occur between femur and the socket. Over time, this contact may lead to inflammation within the hip (synovitis), as well as potential damage to the cartilage within the joint, particularly the labrum, which is a ring of fibrocartilage that lines the rim of the socket.
What are the symptoms of femoroacetabular impingement syndrome?
The primary symptom of FAI syndrome is movement related, or positional related pain in the hip or groin region. However, pain may also be felt in the lower back, buttock or thigh. In addition to pain, patients may also describe stiffness, clicking, catching, locking or giving way.
These symptoms are often felt either during or after vigorous physical activity, such as sports including AFL and soccer, or sports that require a lot of range of movement of the hip, such as dance, gymnastics and calisthenics. However, since symptoms can be related to certain positions of the hip, those who live more sedentary lifestyles can also experience symptoms, for example, when sitting for too long.
Do I have femoroacetabular impingement syndrome?
Just having the features of FAI on x-ray, such as a ‘cam’ or ‘pincer’ lesion does not mean that you have FAI syndrome.
For the syndrome to be present, you must also be experiencing the symptoms of FAI as mentioned above, as well as the ‘clinical signs’ present when your hip is examined by a doctor or physiotherapist, such as reduced range of motion, or pain that is provoked with certain clinical tests.
Other tests such as MRI or CT scan may be required, especially if any surgery is planned. Sometimes, a local anaesthetic injection may be used in the hip may be used to help determine whether your symptoms are arising from within the hip, or from many of the other structures around the hip.
Treatment of femoroacetabular impingement syndrome:
FAI syndrome can be treated by conservative care, rehabilitation or surgery.
Conservative care involves education, monitoring of symptoms over time and lifestyle and activity modification.
Physiotherapy based rehabilitation aims to improve hip stability, hip muscle strength, range of motion and movement patterns.
Surgery, which is usually performed arthroscopically (keyhole), aims to improve the hip joint shape (morphology) and repair any damaged tissue in the hip, such as the labrum (cartilage).
A recently published, large clinical trial in the UK (The ‘FASHIoN Study’), showed positive outcomes from both physiotherapy-led and surgical treatment options for FAI syndrome.
Without treatment, symptoms of FAI syndrome will probably worsen over time. The long-term outlook for patients with FAI syndrome is unknown. However, it is likely that having a cam shape is associated with the development of hip osteoarthritis
Differential diagnosis:
It is important a proper diagnosis is performed, as FAI syndrome must be differentiated from other conditions that may cause hip and groin pain, such as:
- Hip joint instability or hip joint dysplasia (eg. a ‘shallow’ hip socket)
- Gluteal (buttock muscle) tendon problems
- Adductor (groin muscle) tendon problems
- Iliopsoas (hip flexor muscle) tendon problems
- Inguinal hernia
5 tips for self-managing FAI syndrome:
- Avoid sitting in cross-legged positions (especially where one knee is crossed over the other)
- Avoid sitting in positions where the hips are positioned ‘lower’ than the knees, for example, sitting on a low couch. Always try to have your hips higher than the knees.
- When performing stretching exercises for the back and leg muscles, always ensure that you are feeling a good stretch in the desired muscle. If you experience deep hip or groin region pain when stretching, rather than a muscle stretch, this may be counter-productive.
- Avoid excessively deep squats and lunging-type movements.
- If you are a side sleeper, try sleeping with a pillow between your knees to ensure your thigh does not cross over the other during the night
Return to activity:
In patients who are treated for FAI syndrome, symptoms frequently improve, and they return to full activity, including sports.
References:
The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Griffin DR, et al. Br J Sports Med 2016;50:1169–1176.
Need additional help
Our team at Physica are here to help you with all of your musculoskeletal conditions. Please book online using the link in the header or if you have additional questions prior to bookings contact us via email.
Hip Physiotherapists

Clinical Interests
- Low Back + Neck pain and headaches
- Ankle and knee injuries
- Shoulder and elbow conditions
- Post Surgery Rehabilitation
- Tendon injuries
- CrossFit and sporting injuries
- Anything that hurts, really!
To read more about Grant click here

Clinical Interests
- assessment and management of head/neck disorders especially headache
- treatment of neck-related nerve pain
- thoracic spine
- knee pain
To read more about Greg Collis-Brown click here

Clinical Interests
- Neck Pain and Headache
- Low back pain
- Dry Needling
- Post Surgery Rehabilitation
- Sports Injuries
- Shoulder and Knee pain and associated injuries
To read more about Marcus click here

PROFESSIONAL INTERESTS:
- Vestibular conditions i.e. BPPV
- Sporting injuries
- Post-operative rehabilitation
- Foot and ankle
- Shoulders
- Neck and Back Pain
- Dry Needling
To read more about Josh click here

Edward is a recent Master of Physiotherapy graduate, having completed his studies at La Trobe University in 2025. He also previously obtained a Bachelor’s degree in Health Sciences, where he majored in human anatomy and physiology. Edward was also fortunate enough to be selected as a ‘peer mentor’ for the La Trobe anatomy program, where he assisted teaching students in first year anatomy.
Edward has had experience in the sporting setting, where he was a sports trainer for a wide range of local and sub-elite sporting clubs, covering sports such as rugby, AFL football, cricket and soccer. Edward’s deep passion is driven by optimising the health and wellbeing of others, with a particular focus on movement, exercise, injury prevention, and rehabilitation.
Outside of physiotherapy, Edward is dedicated to maintaining a fit and active lifestyle as he enjoys playing AFL football for the ‘Old Yarra Cobras’, going to the gym and spending time with his friends and family, including his golden retriever Rosie.
Clinical interests
• Neck, thoracic and low back pain
• Shoulder pain
• Sporting injuries
• Hip and knee pain
• Ankle and foot injuries
• Pre and Post-operative rehabilitation

Laura graduated from La Trobe University with a Bachelor of Health Sciences/ Master of Physiotherapy in 2015. She completed her post graduate Masters degree in Musculoskeletal Physiotherapy in 2022. Laura additionally has a Bachelor degree in Exercise and Sport Science from Deakin University.
Laura has a special interest in acute and chronic lower back pain presentations. She also enjoys treating hip and knee pain, particularly assessing the biomechanical relationship of these regions and correcting movement dysfunction of lower limb conditions. Following the birth of her son in 2023, Laura has further developed an appreciation for the demands of pregnancy and enjoys supporting women both pre and post-natally.
Clinical Interests
- Acute & chronic low back pain
- Hip & knee pain
- Pre/Post Natal Musculoskeletal Care
- Clinical Pilates
- Biomechanics & Corrective Exercise Therapy

- Low back pain
- Neck pain
- Hip and knee surgical rehab
- Sports Injuries
- Hydrotherapy
To read more about Lachlan click here

Nevine brings over 28 years of clinical experience as a Physiotherapist, including five years as a practice manager. She has specialized in vestibular rehabilitation for 18 years and continence and pelvic floor physiotherapy for 22 years. Her diverse career spans hospitals, private practice, community health, rehabilitation services, and research, including her work on the TELKO study at Melbourne University.
Nevine is bilingual in Egyptian and speaks some Italian, enhancing her ability to connect with clients from diverse backgrounds. Her clinical expertise includes managing spinal and musculoskeletal conditions, shoulder injuries, pelvic girdle and hip pain, whiplash, sports injuries, vestibular and neurological disorders, paediatric care, bladder and bowel health, as well as adult and geriatric rehabilitation.
She is highly skilled in delivering a variety of physiotherapy programs, such as spinal rehabilitation, core stability, Pilates, functional restoration for chronic low back pain, continence rehabilitation, falls prevention, vestibular and balance therapy, and strength training. Nevine uses evidence-based practices and outcome measures to identify the root causes of her clients’ issues, empowering them to reduce pain, stiffness, weakness, leakage, and dizziness, and improve their overall strength, mobility, and balance.
Clinical Interests/Special Interests
- Vestibular Rehabilitation: Nevine has completed extensive vestibular training, including three vestibular certifications and an intensive competency-based course at Monash University. She uses advanced tools like Frenzel goggles to assess and treat conditions such as BPPV, vestibular neuritis, migraines, and balance disorders.
- Continence and Pelvic Floor Physiotherapy: With a Postgraduate Certificate in Continence and Pelvic Floor Rehabilitation from Melbourne University, Nevine helps clients manage bladder and bowel conditions, pelvic organ prolapse, and post-surgical recovery.
- Musculoskeletal and Ante/Postnatal Care: She supports clients with pelvic girdle pain, sacroiliac joint dysfunction, lumbosacral instability, diastasis recti, and perineal tears.
Nevine is dedicated to educating and empowering her clients, helping them achieve better health and well-being through personalized care.

Andrew, a recent physiotherapy graduate, is driven by a deep passion for coaching, human movement, and development. Guided by values of faith, integrity, and respect, he is committed to empowering individuals for optimal functionality, well-being, and personal growth.
Andrew’s diverse background as an athlete and electrician informs his resilient and enthusiastic approach to overcoming challenges and embracing personal development. Grateful for opportunities, he maintains a growth mindset to make a positive impact on the world.
Beyond his professional pursuits, Andrew is a multifaceted individual. Engaging in research and analysis, he stays informed and continuously expands his knowledge. An avid enthusiast of yoga and pilates, he incorporates these practices for solace and rejuvenation. Surfing serves as his active meditation, providing both a physical outlet and a means of staying connected with loved ones through socializing.
Clinical interests:
- Spinal conditions
- Sporting injuries
- Neck and Lumbar pain
- Mid back pain

Tonya completed her undergraduate degree at Monash University and her Master’s degree in Musculoskeletal Physiotherapy at La Trobe University in 2022. Throughout her physiotherapy career, she has worked in both private practice and the public hospital setting, treating patients across the continuum of care from acute injuries to post-operative rehabilitation. Her particular interest is in low back pain.
Prior to studying physiotherapy, Tonya completed an honours degree in Contemporary Dance at London Contemporary Dance School, performing thereafter as a professional ballet dancer. She also ran her own Pilates studio in the UK for 6 years and has been a Pilates teacher to physiotherapists with the APPI. As a result, she has had a lasting affinity for dance and performing arts and was fortunate enough to gain work experience with The Australian Ballet during her studies.
Tonya’s main interest outside of physiotherapy is running. She has completed numerous half and a full marathons.
Clinical Interests
- Neck pain
- Thoracic and Low back pain
- Hip and knee pain
- Shoulder conditions.

Clinical Interests
- Hip conditions – impingement, labral tears, dysplasia and post surgery rehab (joint replacement and arthroscopy).
- Shoulder conditions
To read more about Daniel Zwolak click here

Clinical Interests
- Hip, groin and buttock pain
- Pre and post-operative hip rehabilitation
- Lumbar spine and pelvic pain
- Knee arthritis
- Clinical Pilates
To read more about Leesa click here

Clinical Interests
- sports injuries (basketball & athletics)
- NBL1 Physiotherapist for Ringwood Hawks
- Shoulder- rotator cuff injuries, shoulder replacements, shoulder dislocation management
- Tendon dysfunctions – Achilles, shoulder
- Low back pain
- Elbow injuries (Tennis and holders elbow)
- Lower limb injuries, including ankle & knees
To read more about Matt click here

Feroz graduated from La Trobe University with a Bachelor of Applied Science and his Master of Physiotherapy Practice in 2019.
Feroz has a passion for all areas of musculoskeletal physiotherapy, particularly with sporting injury management and rehabilitation. He has a special interest in neck & back pain, shoulder pain, knee and ankle conditions, post-operative rehabilitation and hydrotherapy.
Feroz believes in a combination of manual and exercise-based therapy along with education and evidence-based practice when treating patients. He also believes in patient-centred care and providing tailored treatment plans based on each individual’s specific goals and lifestyle.
Beyond his professional life, Feroz loves playing footy, basketball, golf, going to the gym and spending time with his family and friends.
Clinical Interests
- Neck, thoracic and lower back pain
- Shoulder Pain
- Knee and Ankle Injury
- Post-operative rehabilitation
- Hydrotherapy
- Clinical Pilates / Exercise therapy
To read more about Feroz click here

Clinical Interests
- Neck pain and headaches
- Jaw (TMJ) injury
- Knees injuries
- Injuries of the foot and ankle
- Low back pain
To read more about Andrew Seymour please click here

SPECIAL INTERESTS
- Neck, mid-back and low back pain
- Pre and Post Concussion management
- Headache associated disorders
- Sports biomechanical assessments
- Complex back, hip pelvic & groin disorders
- Pre and post-surgery rehab
To read more about Anthony please click here

Clinical Interests
- Chronic & recurring back pain
- Sports injuries
- Shoulder rehabilitation
- Exercise programs incorporating Pilates
- Level 1 Lymphoedema Practitioner
- Certified PINC & STEEL Cancer Rehabilitation Physiotherapist.
To read more about Trish click here

“As a Remedial Massage Therapist Carla is passionate about holistic healing and wellness, she brings expertise in remedial massage therapy to help clients alleviate pain, restore mobility, and enhance overall well-being.
With a keen focus on personalised care, she will tailor each session to address individual needs, drawing from a blend of techniques to promote relaxation, release tension, and facilitate healing. Her goal is to empower clients to take an active role in their health.
Injury rehabilitation, postural correction, headaches, muscle or joint pain, sciatica pain and disc degeneration are just a few of the conditions Carla can help with by conducting a thorough postural assessment, hands on treatment and corrective exercises / postural advice.
Carla uses various massage therapy methods and techniques; these include but are not limited to:
- Sports Massage
- Remedial Massage
- Trigger Point Therapy
- Myofascial Release Techniques
- Muscle Energy Techniques
- Relaxation Massage

Clinical Interests
- Dance physiotherapy
- Pre-pointe assessments
- Ante/post-natal musculoskeletal concerns and exercise
- Hip pain
- Clinical Pilates and exercise
- Pre/post operative rehab. (hip and knee)
To read more about Miranda click here

Clinical INTERESTS
- Persistent neck and low back pain
- Hip, groin and pelvic girdle pain (gluteal tendonitis and hip bursitis)
- Headache associated disorders
- Patellofemoral conditions
- Hand therapy
To read more about Chris click here

Clinical Interests
- Neck, middle and low back pain
- Shoulder pathologies
- Sports injuries
- Hip, knee and ankle injuries
- Pre and Post-operative rehabilitation
- Tendon pain
To read more about Alexander click here

Ben recently completed his Master’s in Physiotherapy at Swinburne University in 2024, following a comprehensive educational journey that began with a Bachelor of Exercise and Sport Science, focusing on Exercise Physiology and Strength & Conditioning, at Deakin University in 2020. With a deep-seated passion for sports and human performance, Ben has accrued considerable experience in strength and conditioning, working closely with athletes across various levels—from grassroots to sub-elite—in sports such as AFL and basketball.
His professional journey is driven by a commitment to assist individuals in their recovery and rehabilitation processes, helping them return to their daily activities and sports with renewed vigor and improved function. Ben’s approach to physiotherapy is holistic, considering each individual’s unique circumstances and goals, which allows him to tailor recovery programs effectively.
Ben’s clinical expertise spans a wide range of musculoskeletal disorders and sports-related injuries. His special interests include:
- Shoulder and Scapular injuries: Employing the latest research-based techniques to manage and rehabilitate shoulder complexities.
- Hip, Knee, and Ankle injuries: Focusing on biomechanical assessments and personalized treatment plans.
- Neck, Thoracic, and Low Back Pain: Providing interventions that address both acute and chronic conditions.
- General Sporting Injuries: Offering acute care and preventive strategies to keep athletes at peak performance.
- Strength and Conditioning: Designing programs that enhance physical capacity, improve sports performance, and reduce injury risk.
Beyond the clinic, Ben is an avid sportsman, actively participating in AFL, basketball, and cricket. His competitive spirit and personal experiences in sports give him unique insights into the challenges faced by athletes at all levels. In his spare time, Ben enjoys connecting with friends and family and has a budding interest in culinary arts, constantly exploring new recipes and cooking techniques to broaden his culinary skills.
Ben is enthusiastic about contributing to the field of physiotherapy and continuously seeks to update his skills and knowledge to provide the best care possible. His dynamic and proactive approach makes him a valued member of our team, where he is dedicated to helping clients achieve their health and fitness goals.

Lauren completed her Bachelor of Health Sciences and Master of Physiotherapy Practice in 2016.
Lauren believes a combination of exercise prescription, manual therapy and education are essential components of effective Physiotherapy to help you achieve your goals.
Clinical Interests:
- Post-Surgical Rehabilitation
- Hydrotherapy
- Low Back Pain
- Running Injuries
- Exercise Based Rehabilitation
To read more about Lauren click here

- Hip, knee and ankle injuries
- Neck, thoracic and low back pain
- Return to sport
- Sporting injuries
-
Strength and Conditioning
Book online

Special Interests
- Women’s Health
- Neck & back pain
- Football injuries
- Post-op rehabilitation
- Clinical pilates
- Functional training
- Falls prevention
To read more about Sarah Goh click here

In 2018, Maddie successfully completed her studies at La Trobe University, and she is currently pursuing her Masters of Musculoskeletal Physiotherapy at the same institution. Additionally, she has received training in pilates through the Australian Physiotherapy and Pilates Institute (APPI) and consistently incorporates movement principles into her treatment approaches.
Throughout her career, Maddie has been dedicated to working in private practice, prioritizing patient-centered care. Her focus is on ensuring her clients achieve their maximum potential during their rehabilitation process.
Maddie possesses a particular passion for women’s health and specializes in treating spinal conditions, with a particular emphasis on neck pain, cervicogenic headaches, and thoracic (upper back) pain. Her expertise also extends to effectively managing vertigo and handling complex cases involving underlying health conditions.
Beyond her professional life, Maddie enjoys engaging in various activities. She relishes socializing, camping, hiking, and playing netball. Additionally, she has a love for baking. To stay active, Maddie frequents the gym and enjoys long walks with her groodle, Otis.
Clinical interests:
- Spinal conditions
- Neck and Lumbar pain
- Women’s health Neck pain
- Cervicogenic headaches
- Mid back pain
- Vertigo
- Clinical Pilates

Clinical Interests
- Spinal and hip conditions
- Headaches and TMJ (jaw) dysfunction
- Rotator cuff disorders
- Adolescent and paediatric clients
- Post Surgical Rehabilitation
- Clinical Pilates
To read more about Carolyn click here

Abbey is a recent Master of Physiotherapy graduate, having completed her studies at Swinburne University in 2024. She has also previously obtained an undergraduate degree in Exercise and Sport Science from Deakin University, and a Certificate IV in Physiotherapy Assistance.
Abbey has years of experience working within the paediatric allied health setting, whilst also as a sports trainer for the EFNL. Outside of physiotherapy, she is dedicated to maintaining an active lifestyle through her passion for middle-distance running and strength training.
Clinical Interests
- Acute sporting injuries
- Paediatric conditions
- Sporting injuries
- Knee and ankle injuries
- Low back pain
