What is causing my knee pain?
The knee is made up of various tissues including bone, muscle, cartilage, tendons and fluid.
When any of these structures is hurt or becomes inflamed they have the potential to produce pain and affect your daily life or sporting activities. Similarly, the knee is prone to growth and alignment issues. The team at Physica are well trained to diagnose and manage your knee pain.
What causes knee pain?
Acute injuries
Acute knee injuries can occur from direct trauma to the knee or by sharp pivoting or twisting movements whilst standing on the injured leg. The main structures damaged in these types of injuries are the ligaments or knee cartilages (meniscus and result in pain, swelling and weakness of the knee.
Ligament strain
Ligaments are short tough bands of fibrous tissue in place to help support and stabilise your knee. Damage to these structures usually occurs from trauma or pivoting movements on the injured leg. If you have any knee pain or feel your knee is unstable after such events, it is important to be properly assessed by your physiotherapist in order to determine the location and severity of the tear to establish a suitable rehabilitation plan.
Meniscal / Cartilage Tear
The meniscus of the knee acts as a cushion and stabiliser of the knee. Unfortunately it does have the ability to be injured with any twisting movements of the knee whilst the foot is planted on the ground. This usually results in the symptoms described earlier as well as clicking noises and catching /giving way with knee movements.
What can a Physiotherapist do?
Management
Patello-femoral joint syndrome
The patello-femoral joint is the joint involving your knee cap (patella) and it can be put under undue stress due to the factors discussed above. This stress may result in pain in the area during activities such going up /down stairs, doing squats or even running, and is a common source of pain and dysfunction in many up to 20% of the population.
Patella Tendonopathy
The patella tendon joins your knee cap to you shin bone (tibia). Irritation to this tendon is also known as “jumper’s knee” because it is usually associated with excessive jumping on hard surfaces as seen is such sports as basketball and volleyball.
ITB syndrome (Iliotibial band)
This condition usually occurs in athletes who are running or cycling for long distances. Towards the end of our workout we often get tired and fatigued. With fatigue often our running or cycling technique changes and with this change in technique parts of the knee are put under more stress than others. It is when the outside of the knee is put under this stress that the ilio-tibial band can become irritated and then painful.
Physiotherapy is essential in the management of overuse injuries to the knee to establish not only the structures at fault, but also the underlying causes for those specific structures to fail.
Physiotherapists at Physica are able to conduct running and bike assessments to address any biomechanical problems via technique correction or bike set ups. Muscle imbalances can also be treated in a timely fashion via; soft tissue massage, Dry Needling (western acupuncture) and Strength and stretching exercises. Your physiotherapist can also give you the best advice on your training with regard to training surfaces, footwear, and the amount of training to avoid injury
Arthritis
Osteoarthritis is the most common form of knee pain. This type of knee pain builds gradually over a period of years and is often accompanied by stiffness and occasionally joint swelling. There are many things that physiotherapists can help knee arthritis sufferers with but it is important to act early when any knee symptoms arise.
Infra-patellar Fat Pad Syndrome (Hoffa’s Syndrome)
Infrapatellar Fat Pad Syndrome (IPFPS), also known as Hoffa’s disease occurs when the fatty tissue under the knee-cap is pinched between the femur (thigh bone) and tibia (shin bone). The fat pad is located at the front of the knee joint below the patella and sits either side of the patella tendon (tendon from the knee-cap to the shin bone). The fat pad is richly innervated by nerves and blood vessels, hence it can be easily irritated.
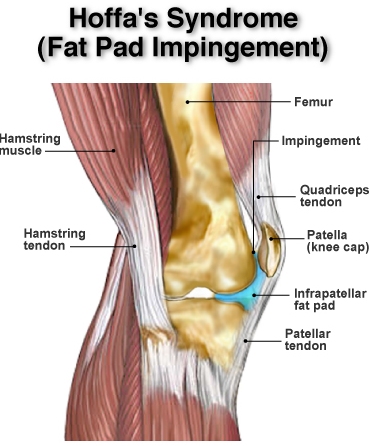
Pain under the knee-cap such as burning or aching is the most common symptom. Activities that straighten the knee or repeated kneeling, repeated jumping and landing can aggravate the condition. Swelling under the knee-cap can be present along with tenderness on palpation.
IPFPS commonly caused by acute trauma, such as falling onto the knee or from knee surgery. Repetitive microtrauma that occurs with biomechanical deficits may also irritate the IPFP. A classic example are patients with ‘squinting patellae’ where the knee-cap faces in, which places undue loading on the IPFP.
IPFPS is usually correctable with physiotherapy. Management involves settling the inflammation with ice, rest and avoidance of aggravating activities. Anti-inflammatory medication may be useful, although a check with your pharmacist prior to commencing this medication is advisable.
Taping the knee to offload and shorten the fat pad is often very successful in reducing pain and immediately improving function. Strengthening of the lower limb musculature such as the quadriceps, gluteals and calf to further offload the IPFP may be indicated. Correction of any biomechanical factors such as foot mechanics, knee and pelvic mechanics is essential. Stretching or releasing tight muscles may also be indicated, especially those around the front and side of the hip.
Severe cases may warrant a cortizone injection and those cases that are not responding may go on to have surgery.
All Physica staff have received training in the diagnosis and management of IPFPS. We will conduct a thorough examination to identify all of your contributing factors and we will devise a step by step plan to return you to optimal health.
Posterolateral Knee Injuries
Posterolateral Corner Knee Injuries
Injuries to the posterolateral corner (PLC) of the knee account for 16% of knee ligament injuries. These type of injuries are complex and frequently overlooked. The posterolateral knee has 28 separate structural components. This complex provides both static and dynamic stability to the knee to prevent excessive hyperextension, tibial external rotation and varus angulation. The three most important stabilising structures of the PLC are the popliteus tendon, popliteofibular ligament and fibular collateral ligament (FCL) (Figure 1).
History
Patients with PLC injuries may present acutely or chronically and often report a mechanism of injury involving sports trauma, a fall or motor vehicle accident. An associated anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) tear are not uncommon due to the similar hyperextension mechanism. Acute injuries present with swelling, posterolateral knee pain and occasionally numbness and weakness in the foot as a result of peroneal nerve disruption.
Examination
The physical examination needs to be thorough to determine if the PLC is involved in your injury. Your physiotherapist will assess the range of movement in your knee, test your strength and palpate specific structures within the knee. They will also perform a number of special tests to provide a better understanding of your injury.
Imaging
Due to the complex anatomy and close proximity of structures imaging may be required. This can assist in identifying specific anatomical structures injured, particularly in acute presentations where the physical examination may be equivocal due to pain and swelling. Magnetic resonance imaging (MRI) is the preferred modality.
Treatment
A conservative approach can be effective and is warranted in less serious injuries. In some cases where the injury is more severe or conservative management has failed to improve symptoms then surgery may need to be considered. Conservative management usually involves a period of immobilization in a brace before commencing a functional rehabilitation program.
Contact one of clinician if you have PCL or posterolateral knee injury




