WHAT IS FROZEN SHOULDER?
Frozen shoulder is a condition is characterised by a progressive stiffness of the joint and pain (Dias, Cutts, & Massoud, 2005). Frozen shoulder is also termed ‘adhesive capsulitis’; whilst this term is still commonly used, it is scientifically inaccurate as there are no capsular adhesions (Yuan, Zhang, & Li, 2017). Rather, frozen shoulder is associated with multi-regional synovitis and contracture of the capsule (Dias et al., 2005). There are some studies that question the presence of inflammation of the joint (synovitis) and rather describe a focal vascularity and synovial angiogenesis (increased capillary growth) (Dias et al., 2005; Yuan et al., 2017). The natural progression of frozen shoulder involves three clinical phases (Dias et al., 2005; Kelley et al., 2013):
Phase I: Freezing – a period of worsening pain and stiffness in the shoulder
Phase II: Plateau – pain usually decreases; however, stiffness remains
Phase III: Resolution (thawing) – spontaneous increase in shoulder range of movement
On average the condition lasts between 9 and 18 months, though few cases may last up to 3-5 years and some people may not fully regain all their range of movement (Dias et al., 2005; Kelley et al., 2013).
Frozen shoulder comes on insidiously, meaning there is no sudden mechanism that causes the injury; it is also an idiopathic condition, meaning the causes are currently unknown. However, research into frozen shoulder provides us with an understanding of risk factors that may lead to a more likely development, they include (Milgrom et al., 2008):
- Diabetes (Type I or II)
- Thyroid disorders
- A prolonged period of immobilisation (i.e. after a shoulder operation)
- A recent fall or injury to the shoulder
The peak age for developing a frozen shoulder is approximately 56; it rarely occurs in people under the age of 40 (Dias et al., 2005; Kelley et al., 2013). Women are more likely to develop it than males, and the non-dominant shoulder is slightly more likely to be affected (Milgrom et al., 2008). A previous episode of frozen shoulder increases the risk of developing the condition on the opposite side (Kelley et al., 2013); however, once resolved recurrence on the same side is unusual (Dias et al., 2005).
CLINICALLY RELEVANT ANATOMY OF THE SHOULDER
The shoulder joint is made up of two joints: the acromioclavicular (AC) joint and the glenohumeral joint. For the purpose of this article, the AC joint will not be explored as frozen shoulder only pertains to the glenohumeral joint.
The glenohumeral joint is a synovial, ball and socket joint formed from the articulation of the glenoid cavity (socket) and the head of the humerus (ball). The articulation ratio is approximately 1:4, meaning the glenoid cavity only covers a small portion of the head of the humerus; this allows for greater mobility than other joints but sacrifices stability. Both articulating surfaces are covered with hyaline cartilage, as with most synovial joints.
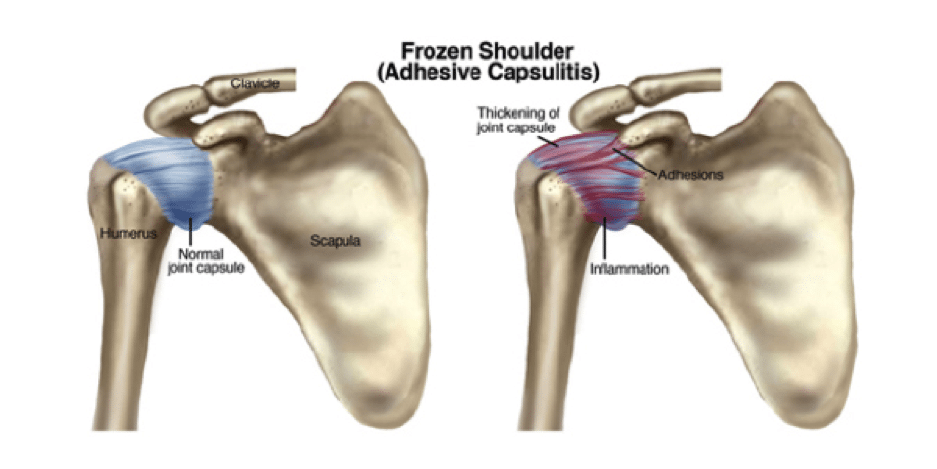
ANATOMICAL IMAGE OF THE SHOULDER AND CAPSULE
The joint capsule (outer layer) is comprised of fibrous connective tissue that extends from the anatomical neck of the humerus to the outer rim of the glenoid. This capsule is formed by the superior, middle and inferior glenohumeral ligaments and it functions as the main stabiliser of the glenohumeral joint. The coracohumeral ligament, extending from the coracoid process to the greater tubercle of the humerus, supports the superior aspect of the joint; thickening of this ligament plays a role in the restricted range of movement in cases of frozen shoulder. The synovial membrane lines the inside of the joint capsule producing synovial fluid to reduce friction during movement.
WHAT ARE THE SIGNS AND SYMPTOMS OF FROZEN SHOULDER?
Frozen shoulder typically presents with a gradual and progressive onset of pain and shoulder stiffness. Pain is commonly felt at the end of range of movement of the shoulder via the mechanism of stretching the capsule (Kelley et al., 2013). Pain can also be prominent at night.
The pain usually presents as a poorly localised deep ache, which may radiate down the anterior or lateral upper arm. Pain is associated with restricted active and passive range of movement at the shoulder. Initially, loss of external rotation (turning the arm out) is most common, followed by internal rotation, abduction and elevation (Dias et al., 2005). The pain and/or restriction results in increasing difficulties with functional activities such as hanging washing out to dry, drying/washing hair and doing up a bra.
DO I HAVE FROZEN SHOULDER?
Diagnosis of frozen shoulder is primarily made via clinical examination; however, imaging studies can be incorporated to exclude other shoulder conditions (Li et al., 2011).
The clinical criteria for the diagnosis of frozen shoulder includes (Kelley et al., 2013):
- Pain for at least one month;
- Pain at night;
- Inability to lie on the affected shoulder;
- Restriction in all passive and active ranges of movement;
- Pain is reproduced at the ends of the patient’s passive range of movement; and
- External rotation is most limited, particularly in adduction.
Imaging studies such as ultrasound (US) and magnetic resonance imaging (MRI) can identify coracohumeral ligament and joint capsule thickening, which is suggestive of frozen shoulder (Li et al., 2011). However, these signs may not be seen until later into the development of this condition (Yuan et al., 2017). Radiology is more useful in this condition to rule out the presence of other possible conditions, such as glenohumeral arthritis (Dias et al., 2005).
TREATMENT OF FROZEN SHOULDER
Current evidence suggests the most effective management for individuals with frozen shoulder is via a combination of medical and physiotherapy management (Cho, Bae, & Kim, 2019). Current evidence for medical management has demonstrated that hydrodilatation can provide significant improvement in individual’s pain and range of movement. This procedure involves the injection of saline solution and corticosteroid into the patient’s glenohumeral joint to help stretch the fibrous shoulder capsule (Cho et al., 2019). There is evidence that a combination of physiotherapy and hydrodilatation is most effective compared with either treatments in isolation (Cho et al., 2019). There is some evidence for the use of corticosteroid injections, however, the evidence suggests it is effective in reducing pain in the short-term but is no different than a wait-and-see approach in the long-term (Cho et al., 2019). CSI treatment seems to only be effective in the long-term in combination with physiotherapy management (Cho et al., 2019; Kelley, McClure, & Leggin, 2009). Though, the evidence suggests a more superior effect is seen in the use of hydrodilatation.
Physiotherapy management involves a combination of pain education, shoulder stretching and glenohumeral joint mobilisation techniques and home exercises (Chan, Pua, & How, 2017; Kelley et al., 2009; Kelley et al., 2013). Exercise programs vary enormously depending on the individual and their goals. For example, the exercise programs for people returning to recreational sport compared to those aiming to perform normal daily functions are understandably different. Though, most programs involve stretching exercises aimed at restoring capsular flexibility and shoulder range of movement (Kelley et al., 2009). Strengthening exercises may also be incorporated into the exercise regime as the surrounding muscles, e.g. the rotator cuff, often becomes weak due to prolonged periods of pain and reduced shoulder mobility.
Intervention may also be aimed at managing other regions that may become affected, for example, biomechanics of the scapula-cervical region are usually altered due to the limited glenohumeral (shoulder) range of movement, this may result in increases to the neck and upper back pain (Kelley et al., 2013).
In some cases of frozen shoulder, where there appears to be minimal to no resolution of movement restrictions over long periods of time, surgical intervention may be appropriate (Dias et al., 2005). A common procedure, which technically involves no surgery, is called manipulation under anaesthetic (Dias et al., 2005; Kelley et al., 2009; Kelley et al., 2013); this involves the forced movement of the shoulder to stretch and tear the capsule while the patient is under anaesthetic, in hopes to ‘kick-start’ improvements in therapy. Another procedure used is termed a ‘capsular release’ performed via arthroscopy. This operation involves the cutting and release of tight portions of the capsule (Cho et al., 2019; Dias et al., 2005); there are understandably more risks involved with this type of procedure, which is why it is usually utilised in cases failing other conservative forms of management.
DIFFERENTIAL DIAGNOSIS
Frozen shoulder can be a difficult diagnosis to make in the early stages, particularly when pain is the only presenting symptom. In the early stages, other possible conditions resulting in similar symptoms to frozen shoulder include (Ewald, 2011):
- Rotator cuff tendinopathy
- Glenohumeral osteoarthritis
- Subacromial or subdeltoid bursitis
- Cervical radicular pain
- Biceps tendinopathy
- Acromioclavicular arthropathy
- Autoimmune diseases e.g. rheumatoid arthritis
- Neoplasm
Once the multi-planar passive range of movement restrictions are apparent, the diagnosis becomes clearer, however, glenohumeral osteoarthritis can also result in similar symptoms and should be ruled out via x-ray (Ewald, 2011).
REFERENCES
Chan, H. B. Y., Pua, P. Y., & How, C. H. (2017). Physical therapy in the management of frozen shoulder. Singapore Med J, 58(12), 685-689. doi:10.11622/smedj.2017107
Cho, C. H., Bae, K. C., & Kim, D. H. (2019). Treatment Strategy for Frozen Shoulder. Clin Orthop Surg, 11(3), 249-257. doi:10.4055/cios.2019.11.3.249
Dias, R., Cutts, S., & Massoud, S. (2005). Frozen shoulder. BMJ, 331(7530), 1453-1456.
Ewald, A. (2011). Adhesive Capsulitis: A Review. American Family Physician, 83(4), 417-422.
Kelley, M. J., McClure, P. W., & Leggin, B. G. (2009). Frozen shoulder: evidence and a proposed model guiding rehabilitation. J Orthop Sports Phys Ther, 39(2), 135-148. doi:10.2519/jospt.2009.2916
Kelley, M. J., Shaffer, M. A., Kuhn, J. E., Michener, L. A., Seitz, A. L., Uhl, T. L., . . . McClure, P. W. (2013). Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther, 43(5), A1-31. doi:10.2519/jospt.2013.0302
Li, J. Q., Tang, K. L., Wang, J., Li, Q. Y., Xu, H. T., Yang, H. F., . . . Zhang, S. X. (2011). MRI findings for frozen shoulder evaluation: is the thickness of the coracohumeral ligament a valuable diagnostic tool? PLoS One, 6(12), e28704. doi:10.1371/journal.pone.0028704
Milgrom, C., Novack, V., Weil, Y., Jaber, S., Radeva-Petrova, D. R., & Finestone, A. (2008). Risk Factors for Idiopathic Frozen Shoulder. IMAJ, 10(5), 361-364.
Yuan, X., Zhang, Z., & Li, J. (2017). Pathophysiology of adhesive capsulitis of shoulder and the physiological effects of hyaluronan. European Journal of Inflammation, 15(3), 239-243.
