Colles Fracture:
- Colles fracture refers to a complete break in the distal radius (wrist), often occurring as the result of a fall on an outstretched hand. The angulation and force of the fall causes dorsal ( upwards) displacement of the broken segment, often occurring approximate 2-3cm proximal to wrist, creating a visible deformity. This deformity is referred to as the ‘Dinner fork’ deformity.
- In many cases there is concomitant damage to the ulnar styloid present.
Did you know that about 15% of people will have a Colles' fracture at some point in time!

INCIDENCE RATE:
- Colles fracture is one of the most common fractures seen in the wrist affecting the adult population. The incidence rates increase in the female, elderly population due to the presence of osteoporotic changes affecting bone strength (Jantzen et al., 2016).
- Children who present with a Colles fracture are often involved in more high impact trauma such as a fall from a tree, horse, bike etc.
Signs and Symptoms:
- pain
- swelling
- deformity
- bruising
COMPLICATIONS:
Patients frequently recover well and return to normal levels of function at approximately 12-16 weeks following this injury however some possible complications are:
- Damage to the median nerve – Patient may present with numbness, pins and needles, ongoing/ progressive muscular weakness.
- TFCC tear- The distal ulna attaches to a meniscus-like structure, the triangular fibrocartilage discus, which can be torn with wrist fractures. This disc acts similarly to meniscus in your knee and helps to absorb load at the wrist, and allow for smooth articulation of the joint.
- Scapholunate dissociation - As a result the impact and displacement of the bone segment the scapholunate ligament can be torn resulting in possible wrist instability.
- Malunion (incomplete bony healing.)
- Repeat Xrays are recommended at one, two, and six weeks to verify proper healing.
- Radius shortening as a result of the impaction trauma
- Reduced range of movement and ongoing stiffness of the wrist joint
RISK FACTORS:
- Osteoporosis – The association between Colles fracture and osteoporosis is so strong that it is encouraged that patients presenting with this injury should have their bone density checked, due to increased risk of other fractures such as the hip ( Jantzen et al., 2016).
- Females – post menopausal.
- History of previous falls/ high falls risk
DIAGNOSIS:
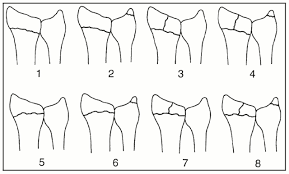
A Colles fracture is diagnosed using plane X-ray. The Frykman classification system is often used to determine the grade of injury.
Frykman classification
SURGERY:
Colles fractures require relocation of the distal radius which can be achieved through casting alone or for more severe grades surgical fixation. The most common surgical intervention is the Open reduction internal fixation (ORIF), which involves the reduction and relocation of the facture site then securing of the bony segments using screws, plates or wire.
PHYSIOTHERAPY MANAGEMENT:
Following surgery or casting physiotherapy management is required for pain reduction and restoration of function. Rehabilitation is separated into three key components:
- Restoring range of movement ( 1-6 weeks)
- Soft tissue release
- Swelling and pain management
- Range of motion exercises for fingers/ hand, elbow and shoulder. Introducing wrist as tolerated and guided by surgical guidelines.
- Gentle active assisted stretching and mobility exercises
- Strengthening ( 6-12 weeks)
- Progressive strengthening program for wrist stability including forearm muscles and intrinsic muscles of the hand ie, grip strength.
- Progression of range of motion exercises and introducing weight bearing stretching
- Functional rehabilitation – Returning to normal hobbies/activities ( 12-16 weeks)
- Task specific exercises
- Increasing strengthening exercises incorporation more functional and kinetic chain movements of shoulder.
- Gradual reintroduction in hobbies/activities.
- Addressing any additional soft tissue injuries/ instabilities
