Anterior Cruciate Ligament
(ACL)
What is the ACL?
What causes an ACL tear?
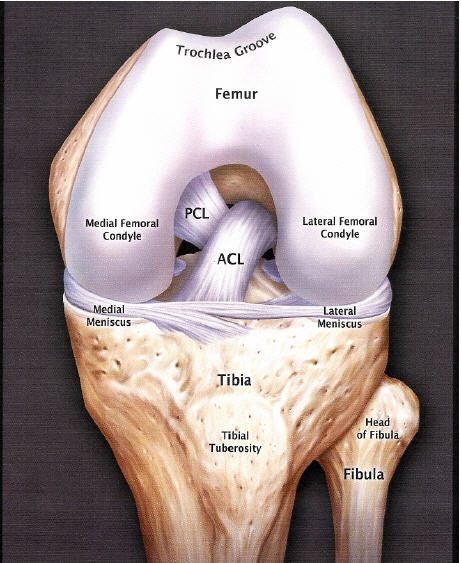
Anatomy of an ACL
Accurate testing of the other structures in the knee are an essential component. It is essential that we cofirm the status of the other main ligaments and structures of the knee. I many cases an ACL tear may be associated with a medial or lateral ligament tear, bone bruising, mensical injury or fracture. In children it is essential that a plain film xray is ordered even prior to an MRI to ensure that a bone fragment has not been avulsed with the trauma.
VIRTUAL DISSECTION OF ACL (Interactive)
Image- http://www.reelshub.com/
Do all ACL injuries require surgery?
No not all people who tear their ACL require surgery. In some cases people can return to their normal lives without an ACL. The decision on whether to have surgery depends on several factors.
Age
In most cases younger people (10-50 years old will undergo surgery.
Activity Levels
The research shows that people who require a higher level of activity from their knee will do better with an intact ACL than a deficient ACL knee. It is for this reason that most surgeons and health professionals will recommend ACL surgery.
General Health
Surgery always has risks associated with it. Other medical issues can increase these risks. Consideration of all other medical factors will play an important role in deciding whether the benefits of an ACL reconstruction out way the risks.
Previous Knee operations
In some cases previous knee surgery or trauma may limit the ability to have a reconstruction. Your surgeon will discuss this with you.
Multi trauma to the knee
Often the ACL does not tear in isolation. If your knee has had a meniscal or a collateral ligament tear then often this will also require surgery. In many cases the presence of other trauma will increase the likelihood that you should consider surgery
What are the symptoms of an ACL tear?
Common symptoms of an ACL strain include
- Swelling
- Inability to weight bear
- Feeling of instability
- Bruising
- Tenderness to touch
- Weakness
- Limited ability to run, kick or accelerate
The grade of the tear will determine the severity of the symptoms. In mild cases, an athlete may continue to play for the rest of game and only feel pain when they have cooled down. With larger tears, the individual may no longer be able to participate in the activity and may even have trouble walking.
How is an ACL tear diagnosed?
All Physica staff are expertly trained in assessing and treating ACL and PCL injuries. The key to an early return to sport is an accurate diagnosis with implementation of sports specific rehabilitation.
The testing of an ACL injury requires skilled manual testing to assess the laxity/absence of the ACL. We use a combination of several tests:
- Pivot shift
- Anterior draw test
- Lachman’s test
- Lift up test
Should one or more of these tests suspect a partial or full tear of the ACL then an MRI is usually ordered.
Immediate management and treatment of an ACL injury involves the RICER protocol (rest, ice, compression, elevation and referral). At Physica, our physiotherapists can detect the extent of an ACL injury with speci c tests and give advice
on management thereon. An MRI is used to con rm the diagnosis.
Treatment of an ACL injury generally involves surgical repair by an orthopaedic surgeon normally completed under general anaesthetic. The surgeon may use the “key-hole” (arthroscopic) method, which uses a camera to look inside the knee. They will make one or more small incisions in your knee and replace the ACL with a suitable graft either from the patella tendon or more commonly from the hamstring.
Rehabilitation following surgery is crucial to the recovery
of your knee. The rst stage involves controlling swelling, regaining full knee extension and restoring quadriceps
(thigh muscle) function. The second stage involves further developing quadriceps, hamstring, calf and gluteal strength. In the third stage speci c functional re-training tasks such as running drills, agility and balance will be incorporated into the program for patients wanting to return to sport. Returning to competitive sport normally takes 12 months.
How are ACL tears treated?
Acute Management 0-48 hrs
Initially, the RICE principles should be applied in the first 48-72 hours:
Rest – Rest from activities that cause pain
Ice – Ice the affected area 20 mins every 2 hours
Compress – Use a compression bandage to minimise swelling,
Elevate – Elevate the lower limb to minimise swelling
Treatment
In many cases surgery is indicated. The role of the Physiotherapist prior to surgery is to minimise swelling and maximise knee range of motion. This often results in a better surgical outcome.
In patients where surgery is not indicated gentle exercises can be commenced soon after the injury occurs. Rehabilitation will include a range of manual techniques as well as strengthening, stretches, sport specific drills and a graded return to sport or activity. Strengthening of the muscle is essential to enable and optimal recovery and these exercises are progressed as the muscle heals.
Rehabilitation
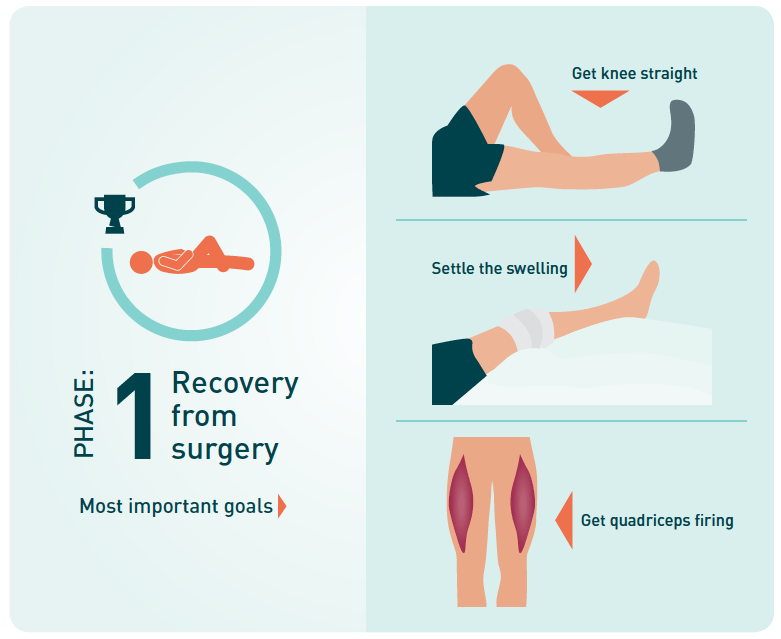
Phase 1- Recover from surgery
weeks 1-4
Goals of Phase 1
1. Attain full knee extension or straightness
2. Control your knee swelling
3. Start training the quadriceps muscles
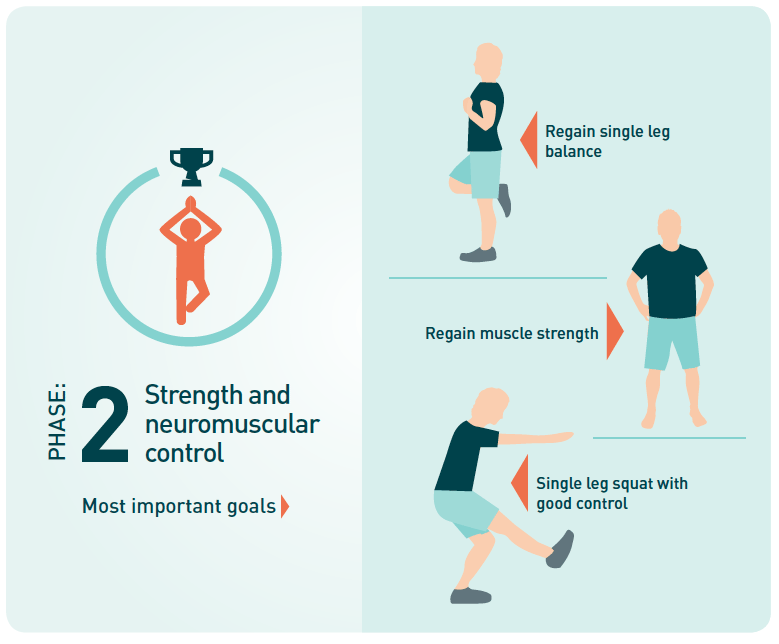
Phase 2- Stength and control
Goals of Phase 2
1. Regain most of your single leg balance
2. Regain most of your muscle strength
3. Single leg squat with good technique and alignment
Phase 3- Running and agility
Goals of Phase 3
1. Score ‘excellent’ on a jump-rebound task
2. Progress successfully through an agility program
3. Regain full strength and balance

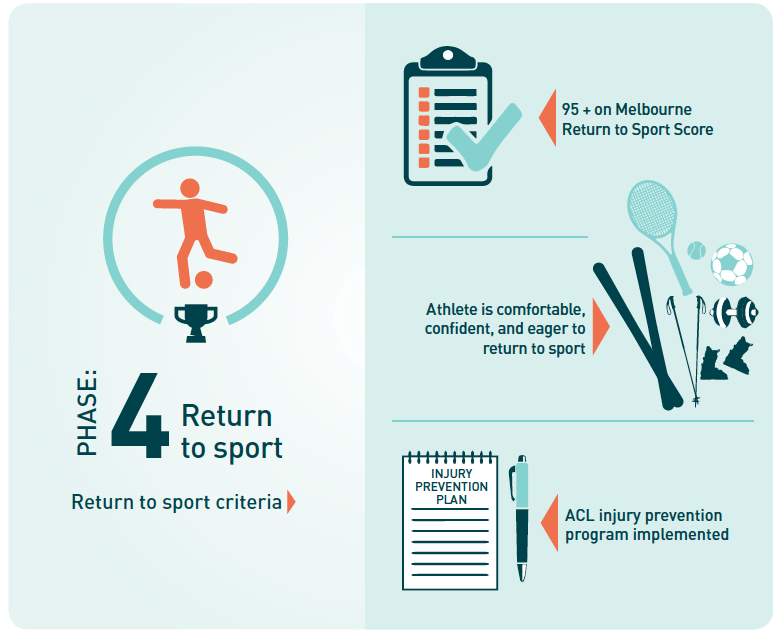
Phase 4- Return to sport
Goals of Phase 4
1.Successful completion of the Melbourne Return to Sport Score (>95)
2.The athlete is comfortable, confident, and eager to return to sport
3.An ACL injury prevention program is discussed, implemented, and continued whilst the athlete is participating in sport
Phase 5- Prevent Reinjury
Weeks 1-4
Goals of Phase 4
1.Successful completion of the Melbourne Return to Sport Score (>95)
2.The athlete is comfortable, confident, and eager to return to sport
3.An ACL injury prevention program is discussed, implemented, and continued whilst the athlete is participating in sport
Phase 5- Prevent Reinjury
-
01
Your Physiotherapist will advise you as to when you are safe to return to sport/activity.
-
02
You can speed things up by an accurate rehabilitation program. Your Physiotherapist will provide you with exercsies and a management plan.
-
03
If you do not have a Physiotherapist download a program below and contact uswith any questions you may have?
How do I make an appointment?
Walking With Crutches
Stand on your good leg with your elbow crutches by your side.
Place your elbow crutches, one at a time, approximately a foot in front of you.
Hop your good leg onto the imaginary line between the two crutches.
Continue this sequence, keeping your gaze directly ahead.
This will be covered in more depth in your week 1 day 1/2 Physitrack app.
Climbing Stairs with Crutches
Walking up stairs:
Stand at the bottom of the stairs.
Hold on to a rail and use elbow crutches as needed.
When going up the stairs, follow this sequence:
– place your good leg on the step first
– next, bring your other leg to the same step
– finally, bring your crutch up to join your feet on the step.
Repeat this sequence for each step until you reach the top.
Walking down stairs:
Hold on to a rail and use elbow crutches as needed.
When going down the stairs, follow this sequence:
– place your crutches on the step you are going to move down to
– next, put your weakest leg down on the same step
– finally, bring your other leg to the same step
Repeat this sequence for each step until you reach the bottom.


Swelling Management
Should I expect swelling?
How do i manage swelling
Shoe advice post ACL
After ACL surgery you will typically be able to weight bear on the leg as tolerated. This may require the use of crutches over the first 1-2 weeks. In order to have the best support while working it is advised you wear supportive lace up shoes to ensure the shoes do not slip.
If you have limited knee range, you may decide to wear a supportive slip on shoe or loosen all the laces of the shoe to provide greater room to place your foot in. A shoe horn may also be of assistance.
Wound Management post ACL
After your surgery you will have several small incisions and one longer incision. These may be covered with strips or a bandage. It is important to keep the incision sites clean and dry as they heal to reduce the risk of infection. This is particularly important in the first 1 to 2 days. Once the strips are removed you may wash the knee in clean water and thoroughly but gently dry the knee directly afterwards. It is common to use stitches that are absorbed by your body. You should not need to remove the stitches. If required, your surgeon or doctor will assist removing any stitches.
If you notice the incision becoming red, achy or weeping fluid a visit to your doctor may be required to assess for any infection.
Pain management post ACL
After surgery is it important to adequately control your pain as this helps you to commence your rehabilitation. Your surgeon should discuss with you pain medications that you can take if required. The application of an ice pack to the knee may also assist in managing post- operative pain as well as swelling. An ice pack may be used for 20minutes at a time throughout the day as required. Over the first 2 weeks it is typical to gradually start reducing the amount of pain medication required.